TEACHING PATIENTS ABOUT CARDIOVASCULAR EVENTS
Teaching patients about their health conditions and how to improve their daily lives is an important task for every registered nurse. It can be a rewarding experience when our patients follow our instructions and thus experience improvement in their health condition. In order to develop a teaching plan that will be effective, a number of factors should be considered.
If a patient or her family is not educated on what is required, does not understand the importance or has barriers to self-care, they will not participate appropriately in care. The goal of education and counseling is to help patients and caregivers acquire skills and knowledge to better manage their lives. Patient may have a lack of knowledge which results in nonadherence to treatment plans; misperceptions are common. Patient and caregivers should receive individualized education emphasizing self-care. Elements of education should include recognition of worsening symptoms, use of medications, modifying risk factors, diet, and exercise. Physical, cognitive, social, and financial factors should be taken into account when developing an education plan. Assess factors such as barriers to change, readiness to change and internal motivation. Having the patient or caregiver do return demonstrations is an effective way to assess how well the patient understood her care plan.
The following represents some of the more important points to teach patients regarding some commonly experienced conditions involving their cardiovascular health. The list is presented in short points that will be easily understood by your patients. We hope you will find this information informative and be able to use these points in your nursing practice.
(Smeltzer, Bare, Kinkle & Cheever, 2008).
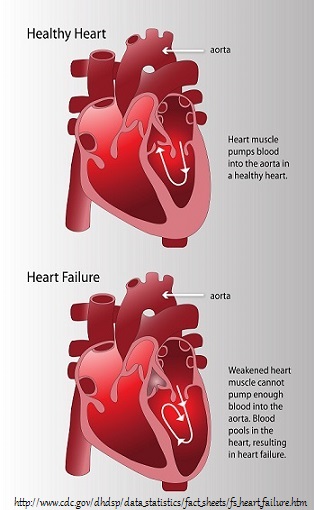
CONGESTIVE HEART FAILURE
- Goal is to help your heart work more easily and not work harder.
- If you experience shortness of breath or swelling in your legs, call your doctor.
- Weigh yourself everyday in the morning on same scale with same amount of clothing on and write down weight – This will show trends in gains or losses.
- Maintain healthy weight – being overweight causes your heart to work to work harder.
- Do not smoke – smoking narrows your blood vessels makes breathing difficult, and decreases the oxygen to your heart which will make it work harder.
- Plan rest periods between strenuous exercise or activities – strenuous exercise puts too much strain on your heart.
- Take your medication every day!
- Try to avoid temperature extremes – your heart works harder trying to keep your body temperature normal.
- Try not to be in the company of others who have a cold or flu – you do not want to become ill.
- Schedule regular appointments with your doctor so that your progress can be monitored.
- Read food labels – many foods contain large amounts of sodium/salt – example is canned soups – choose salt free or low sodium options.
- (Lindenfield, Albert, Boehmer, Collins, Ezekowitz, Givertz, & Walsh, 2010) & (Patient Education Department, 2013)
STROKE
The American Stroke Association has developed the acronym FAST to assist patients in identifying the symptoms of a stroke.
In addition to FAST the patient should also be aware of the following symptoms which could indicate a stroke is occurring:
- Sudden numbness or weakness of the leg, arm or face
- Sudden confusion or trouble understanding
- Sudden trouble seeing in one or both eyes.
- Sudden trouble walking, dizziness, loss of balance or coordination
- Sudden severe headache with no known cause
- (American Stroke Association, 2014)
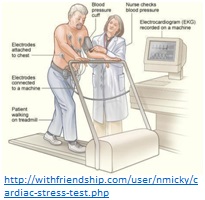
HEART ATTACK AND CORONARY ARTERY DISEASE
Some heart attacks are sudden and intense, but most heart attacks start slowly, with mild pain or discomfort. Often people affected aren’t sure what’s wrong and wait too long before getting help. Here are signs that can mean a heart attack is happening:
- Chest discomfort.
- Most heart attacks involve discomfort in the center of the chest that lasts more than a few minutes, or that goes away and comes back. It can feel like uncomfortable pressure, squeezing, fullness or pain.
- Discomfort in other areas of the upper body. Symptoms can include pain or discomfort in one or both arms, the back, neck, jaw or stomach.
- Shortness of breath with or without chest discomfort.
- Other signs may include breaking out in a cold sweat, nausea or lightheadedness.
- Women can have different symptoms such as: shortness of breath, nausea/vomiting, and back or jaw pain.
- Minutes matter! Fast action can save lives — maybe your own. Don’t wait more than five minutes to call 9-1-1 or your emergency response number. Watch this animation of a heart attack.
Calling 9-1-1 is almost always the fastest way to get lifesaving treatment.
(American Heart Association, 2014)
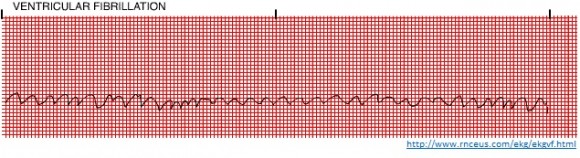
HEART ARRYTHMIAS
Many heart arrhythmias can occur in a patient’s heart. We will provide patient education suggestions for a few of the more common abnormalities.
Atrial Fibrillation
- In this condition, the top chambers or atria of the heart do no contract properly; the atria quiver instead of squeezing which causes pooling of blood in the heart.
- The pooling of blood may cause blood clots which can travel to other parts of the body and cause serious problems.
- Atrial fibrillation can exist for a lifetime or can only be a short term issue.
- Signs of atrial fibrillation include: a heart beat that feels different in some way or fast; feeling tired or weak; feeling dizzy; feeling short of breath; experiencing chest pain; and, possibly nauseated.
- Atrial fibrillation is diagnosed by an EKG.
- One of the most important issues with atrial fibrillation is the prevention of blood clots; patients need to be started on a form of blood thinner to prevent these clots from forming.
- Treatments for atrial fibrillation include: pacemaker; electrical cardioversion (an electric shock is given to the heart which helps it return to a normal beat); and, catheter ablation (wires are fed through an artery or vein to the heart and then the pathway for the abnormal beats is corrected).
- (Patient Education Department, 2013)
Sinus Bradycardia
- Sinus bradycardia is a slower than normal heart rate – usually less than 60 beats per minute.
- This condition can be serious if the heart cannot pump enough oxygen rich blood through the body.
- It can be a normal condition for patients who are athletic or young and healthy.
- Symptoms include: dizziness, shortness of breath, feeling faint or actually fainting, fatigue, and chest pain.
- Sinus bradycardia has many causes. Some of the more common causes are: high blood pressure; heart damage from a heart attack; certain medications; infections and, inflammatory conditions.
- This condition is diagnosed with and EKG.
- Treatments involve changes in medications that may be lower the patient’s heart rate or a pacemaker is commonly used.
- It is important for the patient to tell her doctor if symptoms worsen.
- (Mayo Clinic Staff, 2014)
EKG SHOWING SINUS BRADYCARDIA
Sinus Tachycardia
- ·Sinus tachycardia is a faster than normal heart beat – usually faster than 100 beats per minute.
- Symptoms can be similar to sinus bradycardia and include: dizziness, shortness of breath, rapid pulse, heart palpitations, and chest pain.
- Causes of sinus tachycardia can include: high blood pressure, smoking, fever, drinking too much alcohol or too many caffeinated beverages, side effect of medications, abuse of illegal drugs such as cocaine, imbalance of electrolytes, and overactive thyroid.
- Sinus tachycardia is also diagnosed by an EKG.
- Treatments for this condition include: medications known as anti-arrhythmic drugs such as Rythmol; drugs known as calcium channel blockers, such as Cardizem or beta blockers, such as Lopressor.
- Treatments for can be also include: pacemaker; electrical cardioversion (an electric shock is given to the heart which helps it return to a normal beat); and, catheter ablation (wires are fed through an artery or vein to the heart and then the pathway for the abnormal beats is corrected).
- (Mayo Clinic Staff, 2014)
EKG SHOWING SINUS TACHYCARDIA
NUTRITION FOR YOUR CARDIOVASCULAR SYSTEM
- Eat a variety of nutritious foods from all the food groups such as; fruits, vegetables, whole grains, low-fat dairy products, poultry, fish and nuts, while limiting red meat and sugary foods and beverages.
- Eating a variety of fruits and vegetables may help you control your weight, cholesterol and your blood pressure.
- Eat less of the nutrient-poor foods such as those that are high in calories and low in nutrients like desserts or “junk foods” – chips, Doritos, etc.
- Limit the amount of saturated fat, trans fat and sodium you eat.
- Choose lean meats and poultry without skin and prepare them without added saturated and trans fat.
- Eat fish at least twice a week. Recent research shows that eating oily fish containing omega-3 fatty acids (for example, salmon, trout and herring) may help lower your risk of death from coronary artery disease.
- Select fat-free, 1 percent fat and low-fat dairy products.
- To lower cholesterol, reduce saturated fat to no more than 5 to 6 percent of total calories. For someone eating 2,000 calories a day, that’s about 13 grams of saturated fat.
- Cut back on beverages and foods with added sugars.
- Choose and prepare foods with little or no salt.
- If you drink alcohol, drink in moderation. That means one drink per day if you’re a woman and two drinks per day if you’re a man.
- It is important to watch your portion sizes. Restaurant portions are usually much greater than you might realize.
- Review the following graphics for some additional easy to follow details.
- (American Heart Association, 2011)