Healthcare in the United States is a highly polarizing topic in American politics. Currently, the United States can be characterized as having a pluralistic healthcare system (Shi & Singh, 2010). According to Shi and Singh (2010), the healthcare system in the United States has no central government agency to administer any type of coordinated effort, contains an imperfect delivery system due to imperfect market conditions, government acts as a subsidiary to the private businesses sector, and focused on technology and innovation to provide treatment and care. Finally, according to the authors, unequal access and high costs assists with providing average health outcomes in treatment situation, while failing to focus on the prevention of disease through correct lifestyle behaviors (Shi & Singh, 2010).
Currently, the 115th United States Congress is now attempting to salvage its previous two attempts to overhaul the healthcare system by attempting to replace the Affordable Care Act (also known as the ACA or ObamaCare). One of the key provisions in the new Graham-Cassidy bill would eliminate the federal funding for Medicaid expansion and ACA subsidies (Fox & Mattingly, 2017). Moreover, federal money would be given to the states to determine the best means for distribution to help people pay for their healthcare premiums, while managing high risk insurance pools (Fox & Mattingly, 2017). While the healthcare debate and the future direction will undoubtedly affect everyone, the legislation fails to move away from the contemporary Biomedical Model of Health (Schneider, Fruman, & Coutts, 2005). Currently, the United States if healthcare system focuses on the treatment of illness rather than prevention (Shi & Singh, 2010). As a result, fiscal efforts are driven through treatment and innovative processes to help increase recovery from chronic illnesses but fails to address the wide range of possible causes from a prevention standpoint (Shi & Singh, 2010). For example, if a patient were to be diagnosed with high blood pressure, they would most likely be provided with medication to help reduce blood clotting, which results in the thinning of the blood. However, the patient’s treatment most likely would not center on resolving the behaviors and external variables (determinants) contributing to my high blood pressure. The treatment plan fails to address the patient’s poor dietary habits such as eating high volumes of red meat and fatty laden foods, while excluding consumption of fruits and vegetables. Moreover, it ignores the patient’s lack of regular exercise. How can applied social psychology help intervene and correct my behavior?
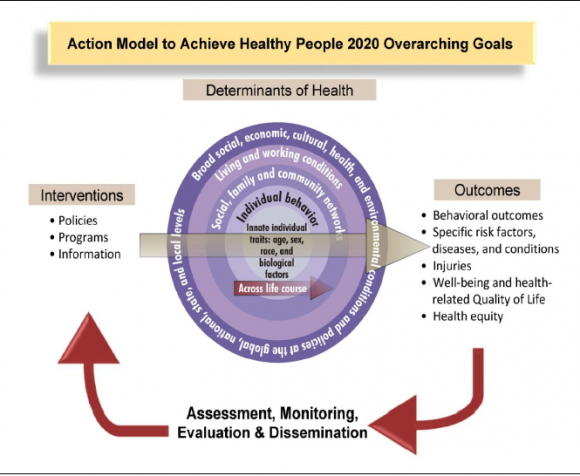
One way applied social psychology can help is through the creation of interventions aimed at correcting the behaviors that are not conducive to a positive health outcome. Additionally, understanding the correct methods of persuasion and social influence can assist with the development of an intervention strategy. One popular alternative to the Biomedical Model of Health is the Healthy People 2020 initiative. The Healthy People 2020 initiative looks at and focuses on the “determinants” of health (Anglin & Blakley, n.d.). Therefore, it focuses on a person’s physical environment, social environment, individual behavior, biology/genetics, and health services, which have a determinate role in a person’s health outcome (Anglin & Blakley, n.d.). Going back to the example, the first step in the intervention would be to determine and identify the problem. In this case, the problem centers on patient’s high blood pressure, which is the result of poor eating and exercise habits. Secondly, a solution will need to be developed. In this case, the solution will be to modify the patient’s eating behaviors and transition to healthy eating and exercise behaviors. Our goal will be to reduce blood pressure levels to prehypertension levels and reduce body mass index (BMI) to correct levels. This will be done through educational information about proper nutrition, assistance with correct meal preparation, and portion control. Education information on proper exercise methods, routines, exercise scheduling, and training will be provided to help assist with meeting exercise goals. The educational information can be presented in a way to attempt to exert social influence over the patient through informational appeals. Using informational appeals allows for social influence through the presentation of the facts or reasons why a health behavioral changes is needed (Schneider et al., 2005). Another method for social influence would be to create a fear appeal, which uses fear arousal as a means to get another person to listen to a message with the goal of creating a behavioral change (Schneider et al., 2005). However, using the fear arousal method should be used at moderate levels in order to prevent the person from ignoring the message (Schneider et al., 2005). All of the suggested activities are designed to improve the patient’s eating and exercise habits in order to achieve the goal. After the goal setting and design phase, the next step will be to implement the intervention, which should happen at a point when activities and target goals have been mapped out chronologically with various time expectations. Finally, the intervention will need to be evaluated for its success and should the intervention not show the desired results, the intervention will need to be adjusted and reevaluated.
In conclusion, while the future of healthcare continues to be debated and remains as one of the most challenge endeavors for policy makers, it is possible to redirect efforts towards focusing on the determinants of healthcare as outlined in the Health People 2020 initiative (Anglin & Blakley, n.d.). Applied social psychology could be a partner of the Health People 2020 initiative by developing interventions designed to address the challenges behind the determinants of health, which could allow for an increase in the amount of positive healthcare outcomes through a prevention centric model rather than a reactionary model of healthcare.
References
Anglin, T., & Blakley, C. (n.d.). Healthy People 2020 and Adolescent Health. Retrieved September 19, 2017, from https://www.hhs.gov/ash/oah/sites/default/files/ash/oah/oah-initiatives/ta/experience_expertise_anglin_blakey.pdf
Fox, L., & Mattingly, P. (2017, September 19). How Obamacare repeal came back with a fury. Retrieved September 19, 2017, from http://www.cnn.com/2017/09/19/politics/obamacare-repeal-is-back/index.html
Schneider, F. W., Gruman, J. A., & Coutts, L. M. (2005). Applied social psychology: Understanding and addressing social and practical problems. Thousand Oaks, Calif: SAGE Publications.
Shi, L., & Singh, D. A. (2010). Essentials of the U.S. health care system (2nd ed.). Sudbury, Mass: Jones and Bartlett Publishers.
United States Department of Health. (n.d.). [Illustration of Healthy People 2020 Initiative]. Healthy People 2020 Initiative. Retrieved from https://www.health.ny.gov/statistics/chac/improvement/hp2020_action_model.htm

Overall, this posting served as an excellent overview of the modern landscape of American healthcare. I felt that you appropriately described the current attempt to overhaul healthcare in America. Additionally, you presented the lingering implications of the Graham-Cassidy bill, in addition to the role that new stakeholders such as state governments would play in healthcare. Perhaps most importantly, I felt that you introduced an important topic regarding the structure of American healthcare. At present, American healthcare does appear to align with the biomedical model of health and illness. Our nation has become increasingly interested in eliminating diseases rather than taking preventative measures (Schneider et al., 2012, p. 168). In your post, you mention that companies remain committed to treatment and recovery programs rather than seizing opportunities to advocate for prevention. However, one must question if capital could be better allocated for intervention processes such as social marketing.
I chose to write about this topic this week as I feel that preventative measures serve a much bigger purpose than simply treating diseases. There must be a push towards behavioral intervention. Ideally, the American healthcare system should be able to balance preventative marketing tactics as well as the continued push for innovation and treatment. However, without prevention, the healthcare system will continue to be overwhelmed by a consistent increase in noncommunicable diseases. Schneider et al. (2012, p. 176) provide an excellent introduction to the health belief model. Of the many components that make up this model, several variables correlate well with your argument favoring social influence. Perceived severity and susceptibility of illness remain two of the most critical aspects impacting the health of Americans (Schneider et al., 2012, p. 176). Many people simply do not feel that they may someday fall victim to a disease. Additionally, individuals remain naïve or unaware of the severity of noncommunicable diseases. It appears that these two variables remain excellent targets for social influence campaigns. Targeting illness severity and susceptibility is only the first step in building a healthcare system based on prevention however. The sheer number of components that make up the health belief model demonstrate the complexity of healthcare overhaul as well as the quantity of situational variables that contribute to the decline of an individual’s health.
References
Schneider, F., Gruman, J., & Coutts, L. (2012) Applied social psychology: Understanding and addressing social and practical problems. 2nd ed. Thousand Oaks, CA: SAGE Publications, Inc.