Beginning well before the pandemic, college students have been facing increased mental health issues. This has resulted in significant change in the needs of college students and a restructuring of priorities and resources necessary to help students thrive.
Students struggle with a variety of mental health issues like depression, anxiety, addiction, eating disorders, and PTSD. In addition to pre-existing mental health struggles that can worsen, students are often commonly affected by social issues such as: academic pressure, discrimination, loneliness, financial issues, insomnia, food insecurity, and social pressures. According to the Cambridge Handbook of Social Problems, “Mental illness is not only in itself considered a major social problem, it also often results from the diverse social problems individuals have to face” (Busfield, 2018).
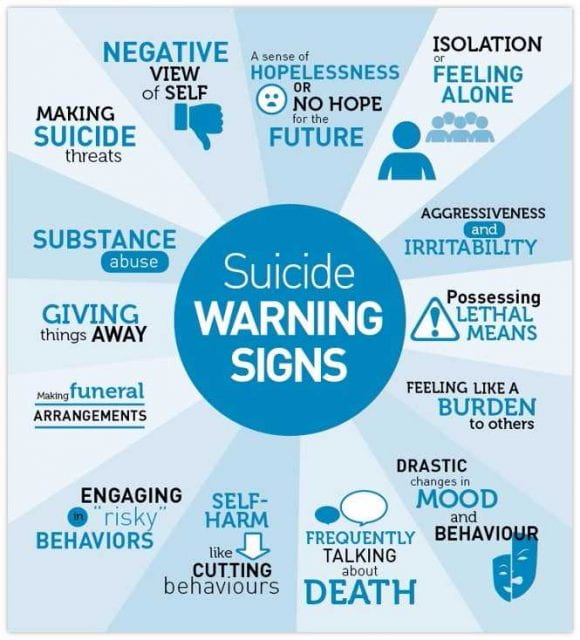
One of the growing needs on campuses is for both mental health awareness and resources. The effect on students and their performance is significant. “Mental health problems can affect a student’s energy level, concentration, dependability, mental ability, and optimism, hindering performance. Research suggests that depression is associated with lower grade point averages, and that co-occurring depression and anxiety can increase this association” (Suicide Prevention Resource Center). Stigma needs to change in terms of how students are perceived and treated. For this to happen, students, faculty, and administration need the resources to build awareness and affect change.
One of the growing resources for college students is the area of on-campus mental health and disability services. Unfortunately, the need often far outweighs the speed at which resources can be developed and offered. One of the resources students can use is disability accommodations, which take into account the impact of mental health on academic performance. Students are then able to counteract some of the negative outcomes usually resulting from mental health struggles such as inability to concentrate and fluctuating dependability. The downfall of this resource is that it requires a medical professional’s diagnosis and significant written, supporting documentation. Therefore, for any student who doesn’t see a professional due to stigma, confusion about how or where to get help, inability to pay for professional help, etc. won’t be able to use this resource as students who don’t face these additional barriers can. This points to a clear problem that needs to be addressed.
Another change that is slowly taking place that is more inclusive than providing academic accommodations is in the area of course structure and assessment strategies. There is a growing trend toward more equitable grading practices in education. This type of grading allows for differences in student performance that aren’t associated with mastery. According to an article in Ed. Magazine by the Harvard Graduate School of Education,“in traditional grading, many commonly used grading categories invite biases. For example, when we include a student’s behavior in a grade, we’re imposing on all of our students a narrow idea of what a “successful” student is”
“In more equitable grading, grades must accurately reflect only a student’s academic level of performance, exclude nonacademic criteria (such as behavior), and use mathematically sound calculations and scales…Grading practices must counteract institutional biases that have historically rewarded students with privilege and punished those without, and also must protect student grades from our own implicit biases.” (Hough, 2019).
Resources:
Busfield, J. (2018). Mental Illness and Social Problems. In A. J. Treviño (Ed.), The Cambridge Handbook of Social Problems (pp.23-42). Cambridge University Press.
“Consequenses of Student Mental Health Issues”. Suicide Prevention Resource Center. https://sprc.org/settings/colleges-and-universities/consequences-of-student-mental-health-issues
Hough, Lory. May 18, 2019. Grade Expectations: “Why we need to rethink grading in our schools”. Ed. Magazine. Harvard Graduate School of Education.