Today the flu virus is nothing more than a seasonal stressor for those who aren’t of vulnerable populations. However, the flu virus of today was not the same flu virus of the 1918 Spanish Flu Pandemic.
The 1918 Spanish Flu was an epidemic of H1N1 flu, a subtype of influenza A. This subtype was particularly infectious and lethal because of a rare combination of 8 genes which made an exceptionally unique natural-born killer. Unusually, the H1N1 flu had a characteristically high death rate amongst healthy adults, ages 15-34 years old. The high death toll was due to the efficiency of viral infection. Once the virus infected the lungs, it would overstimulate the immune system, causing a cytokine storm which encouraged the extensive migration of white blood cells to the lungs.
While this may seem good thing, such an extreme immune reaction resulted in the destruction of lung cells and secretion of blood and mucus into the airway, causing difficulty breathing and suffocation. By the end of the pandemic in April 1920, nearly 500 million people worldwide had been infected and an estimated 17-50 million people died of the virus. The H1N1 flu virus alone lowered the United States life expectancy by more than 12 years. Accordingly, it is considered one of the deadliest pandemics in human history(1).
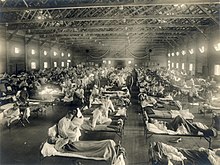
Yet beyond the virulence of the H1N1 flu strain, the spread of the pandemic was largely due to World War I. Such an unprecedented large-scale war led to the drafting of millions of soldiers from countries across the world. Bringing together such a vast population in such unsanitary wartime conditions simply aided the virus’s spread.
Furthermore, the lack of abidance by a strict quarantine procedure within militaries did nothing to mitigate the spread of the virus. In the United States, when Camp Funston in Kansas was experiencing a rapid increase in H1N1 flu deaths, military officials transferred countless soldiers seeking refugee from the virus’s scourge(2). Instead, these soldiers simply brought the H1N1 flu virus with them to the military base they were transferred to. Additionally, soldiers from these infected military bases were being shipped across the Atlantic to fight on the warfront. In doing so, they continued to expose and spread the virus throughout the US military’s ranks and throughout the international militaries(3). However, the virus wasn’t limited to the militaries as the H1N1 flu quickly spread from the military bases to the surrounding citizenry.

Though the greater context of World War I is largely blamed for the H1N1 flu pandemic’s devastation, it was truly the ignorance and disregard of basic epidemiology principles which created the perfect storm that was the 1918 Spanish Flu.