It’s said that intelligence is learning from your mistakes while wisdom is learning from the mistakes of others. For our final dive into pandemics and public health, let’s be wise. Let’s examine the historical mistakes of how pandemics and health crises were mismanaged and apply this wisdom when the inevitable next pandemic arises. There are 3 big take-aways.
1. Unknown Origins of Disease

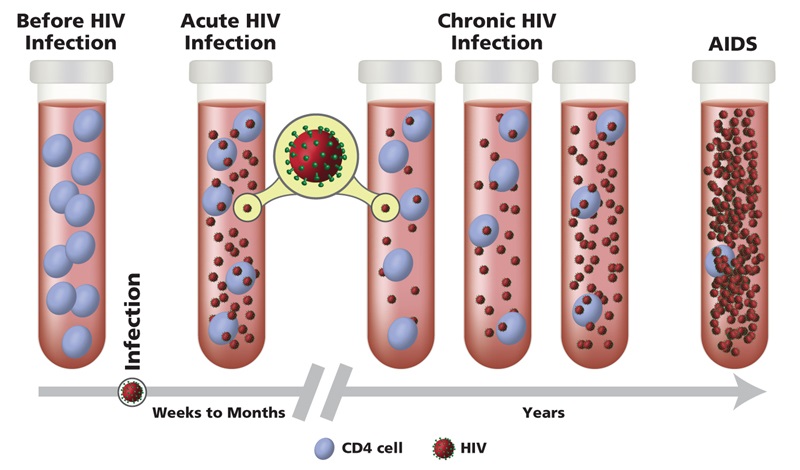
One of the biggest hurdles in combatting an emerging pandemic is not knowing what microogranism is responsible. As the cholera and AIDS pandemics demonstrated, this lacking knowledge leads to the circulation of various theories and speculations which soon become widely accepted as facts. Additionally, the mysterious origins of the disease prevents effective combative strategies against the spread. What type of pathogen determines whether it spreads through the air, water and food, on surfaces, or through a living vector. Without this initial understanding of what’s lurking in the shadows, the process of containing a pandemic is shut down before it can even get started. From this mysterious and therefore frightening origin stems the other hurdles in handling a pandemic. Accordingly, it’s key to establish the pathogen in question and sole means of transmission as early on in a pandemic event as possible.
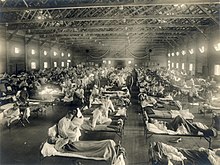
2. Inability to Contain and Isolate the Sick

Another hurdle in combatting a pandemic is the ability to contain and isolate the sick from the healthy, especially those most vulnerable to infection. As the Spanish flu, SARS-CoV-1, and SARS-CoV-2 pandemics exemplify, a failure to isolate and contain the sick and asymptomatic carriers aids the pathogen in propagating rapidly throughout the population, no matter what other combative measures are attempted. Accordingly, once the origin of the disease is established, government and health services must effectively instill an isolation protocol proportional to the contagiousness of the disease. Furthermore, a major and often overlooked population with a high transmission rate is the military. The spread of the Spanish flu is largely attributed to the poor quarantine protocols of world militaries, through which the virus spread from citizens to military to new military to new country. Though it’s important to effectively contain and isolate disease within the general population, these efforts are undermined by decisions to allow various sectors and privileged classes to continue operating as they did prior to the pandemic in question.
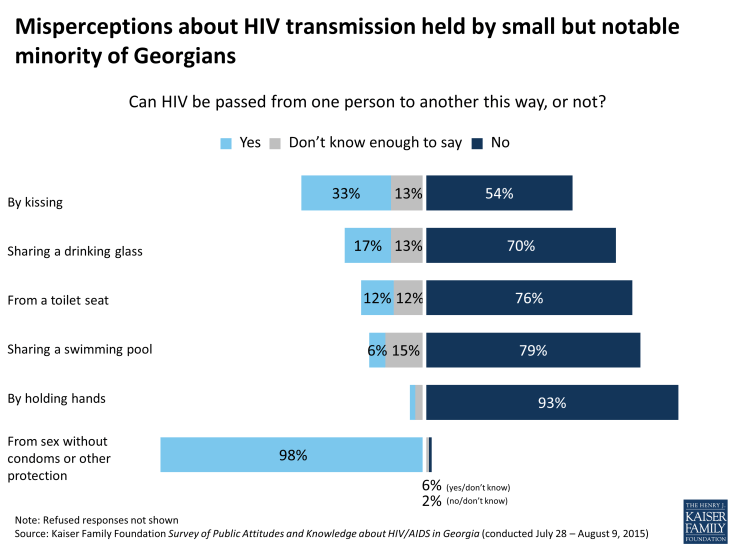
3. Combatting Misinformation and Fearmongering

Finally, the most difficult to manage hurdle is combatting misinformation. Misinformation is a common obstacle, but it becomes especially dangerous at times of intense fear and mass panic, such as pandemics and other public health crises. As the AIDS pandemic greatly highlights, misinformation can spread rapidly, instilling itself in popular belief even after the actual health crisis is long over. From the start of a health crisis, it’s important for governmental bodies to establish open and honest communication with the public. When the public feels that governments are hiding things from them, it sows the seeds of distrust which cause the public to seek out other sources for their information. Americans’ trust in the federal government is always severely low, and this unhealthy relationship gets in the way of a society collectively uniting with the common goal of rooting out disease.
Let’s learn through history and the mistakes of those who came before us. By understanding and tackling these three major hurdles in combatting the spread of infectious disease, we can better manage the inevitable health crises of our future. Don’t just be smart. Be wise!