Often cholera is treated like a disease of the past, grouped together with the plague and smallpox which pose no serious modern concerns. While such an assertion is partially valid in that cholera no longer affects all of the modern world, unlike the plague and smallpox, it’s still prevalent and dangerous.
Cholera is an infection of the small intestine caused by the bacterium Vibrio cholerae. Infection can begin anywhere from 2 hours to 5 days after exposure to the bacterium. Symptoms usually include diarrhea, nausea and vomiting, and dehydration. Due to this symptom profile, cholera can quickly become deadly as the rapid loss of large amounts of fluids and electrolytes can result in death within hours.
In the past 200 years, there have been 7 cholera pandemics, the most recent being the 2016-2021 Yemen cholera outbreak. The third cholera pandemic, occurring between 1846-1860, is most frequently thought of when discussing the dangers of cholera.
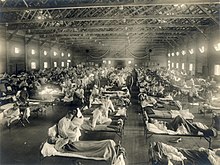
In the 18th century, Great Britain was rapidly industrializing and by the 19th century, London was the largest city in the world due to mass migration from the countryside into industrialized towns. However, the city was unprepared for safely accommodating such large masses of people.
The city quickly became overwhelmed by human waste from the rapidly growing population who largely lived in the squalor of the overcrowded slums. Human waste soon overflowed into the gutters and the waterways. Until the COVID-19 pandemic, it was the worst outbreak in London’s history, claiming over 15,000 lives.

At the time, the origin of the disease was unknown. The widely believed Miasma Theory held that cholera was the result of bad, stale air. Luckily one physician wasn’t so accepting of this theory. After systematically analyzing the people stricken by cholera in Soho, London, Dr. John Snow realized that all patients had one thing in common: a communal water pump. By removing the pump’s handle, the local outbreak ended.
While the solution of clean water seems like an easy fix, safe drinking water is a luxury in many parts of the world. 1 in 4 people worldwide don’t have access to safe drinking water with 6% of deaths in impoverished countries being the result of unsafe water. Each year, unsafe water is responsible for 1.2 million deaths. However, this issue is quickly hitting home in the United States as well.

Fresh water, “the oil of the 21st century” is quickly dwindling in parts of the United States due water stress from major population growth and changes in local climate. Since 2014, the citizens of Flint, Michigan are still without uncontaminated water.
While cholera is one example of diseases spread through contaminated water, other examples include dysentery, hepatitis A, typhoid, and polio. Furthermore, unsafe drinking water exacerbates malnutrition, resulting in childhood stunting which is also an important risk factor for death globally.

For these reasons, maintaining and providing universal access to clean drinking water is a major global health emergency as the human population continues to grow and overwhelm Earth’s renewable resources.
PS. While researching, I discovered that there are two Cholera families in the United States dating to 1920. The last name of Cholera is most commonly found in India and 71% of Choleras live in Asia.